Er zijn geen resultaten gevonden voor jouw zoekopdracht.
Inhoud
U bent succesvol uitgelogd.
Nog niet geregistreerd?
Alternatief voor antibiotica in de wondzorg
De schatting is dat in ontwikkelde landen 1 tot 2 procent van de bevolking gedurende hun leven een complexe wond zal krijgen. De incidentie van complexe wonden neemt snel toe.[1] Wondinfecties kunnen het genezingsproces in gevaar brengen en leiden tot vertraging van de wondgenezing, met een aanzienlijke negatieve impact op de kwaliteit van leven[2,3] Bovendien lopen patienten ook een risico op complicaties zoals een amputatie of een sepsis.[4] Ook hebben geinfecteerde wonden veel impact op de zorgkosten.[2,3]
De frequentie van wondinfecties varieert en is afhankelijk van verschillende factoren, zoals de soort wond, de algehele gezondheidstoestand van de persoon en het onderliggend lijden. Over het algemeen komt een wondinfectie niet bij alle wonden voor, omdat ons lichaam normaal gesproken effectieve afweermechanismen heeft.
Bij kleine acute wonden, zoals kleine snijwonden of schaafwonden, is het risico op infectie vaak lager. Echter, bij grotere wonden, bijtwonden, of wonden die in contact zijn gekomen met vuil, kan het risico op infectie toenemen.
0%
van de complexe wonden is naar schatting geïnfecteerd. [5,6]
0%
van de complexe wonden bevat biofilm met een rol bij wondinfectie. [7,8,9,10]
Complexe wonden
Het continuüm van wondinfecties geeft de verschillende stadia van wondinfectie weer, van initiële besmetting tot een systemische infectie.[11,12] Dit concept kan wondzorgprofessionals helpen de beste strategie te vinden om wondinfecties te voorkomen, te diagnosticeren en te behandelen. Maak kennis met ons behandelconcept voor alle stadia van het wondinfectiecontinuüm:
Prontosan® om de vorming van biofilm te voorkomen en de bacteriële belasting te verminderen, en Askina® Calgitrol, zilveralginaat pasta, dat een aanvullende antimicrobiële activiteit biedt en helpt contaminatie door bacteriën te voorkomen.
De belangrijkste fasen zijn:
Normale genezing. In dit stadium verloopt de wondgenezing normaal zonder tekenen van infectie. Het immuunsysteem en de natuurlijke afweer van het lichaam werken efficiënt om de wond te genezen.
Lokale infectie. Als bacteriën de wond binnendringen, kan er een lokale infectie optreden. Dit wordt vaak gekenmerkt door roodheid, zwelling, pijn en mogelijk pusvorming.
Uitbreidende infectie. Als de infectie niet adequaat wordt behandeld, kan deze zich verspreiden naar diepere weefsels, spieren of botten, wat kan leiden tot ernstigere complicaties.
Systemische infectie. In zeldzame gevallen kan een wondinfectie zich verder verspreiden naar de bloedbaan, wat bekend staat als sepsis. Dit kan levensbedreigend zijn en vereist onmiddellijke medische aandacht.
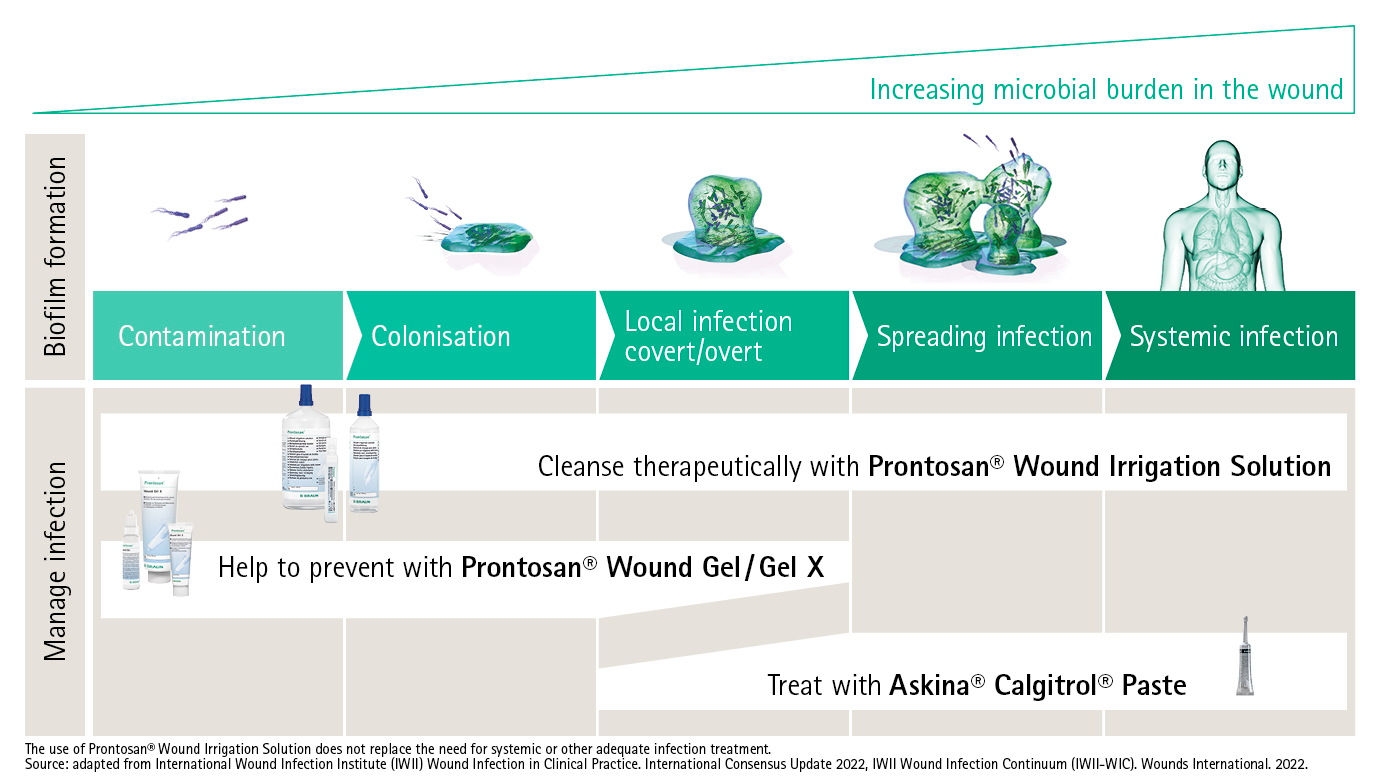
Een grondige wondbeoordeling is van essentieel belang voor het voorkomen en behandelen van wondinfecties en alle mogelijke complicaties.[13,14] De juiste diagnose en productselectie kan je helpen wondinfecties te voorkomen en te behandelen. Prontosan® en Askina® Calgitrol pasta vormen een uitstekende match in de strijd tegen wondinfecties.
De volgende casestudies zijn uitgevoerd om de effectiviteit van een biofilmverwijderaar/-reiniger in gelvorm te beoordelen, Prontosan®, in combinatie met het gebruik van een zilververband , Askina® Calgitrol Paste of Askina® Calgitrol Thin bij patiënten met geïnfecteerde wonden.
Voor alle wonden in het onderzoek werd het volgende behandelprotocol gevolgd:
Alle wonden vertoonden in de eerste week van de behandeling een aanzienlijke vermindering in tekenen van infectie. Ongeveer 50% van alle wondinfecties was in week 2 volledig verdwenen. 80% van alle wonden vertoonde in minder dan 3 weken geen klinische tekenen van infectie meer. Geen van de patiënten kreeg orale of intraveneuze antibiotica tijdens het onderzoek; alle patiënten werden alleen behandeld met lokale antimicrobiële middelen. Er was ook een afname van de geur in alle wonden.
Lees de volledige studieWondinfecties worden veroorzaakt door bacteriegroei in het wondbed. Micro-organismen kunnen op verschillende manieren in het wondbed terechtkomen. De infectie kan leiden tot sepsis wanneer bacteriën zich verspreiden in de bloedbaan, waardoor een levensbedreigende sepsis met multi-orgaanfalen kan ontstaan. [15]
Wondinfectie is een complicatie die je wilt voorkomen omdat de wondgenezing aanzienlijk stagneert.
Lees meer over wondbedvoorbereidingDe pasta sluit naadloos aan op het wondbed en creëert een vochtige wondmilieu wat bevorderlijk is voor natuurlijke genezingsomstandigheden om besmetting door bacteriën te voorkomen. [16]
Lees meer over zilverpastaReferenties
[1] Sen CK, Gordillo GM, Roy S, Kirsner R, Lambert L, Hunt TK, Gottrup F, Gurtner GC, Longaker MT. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen. 2009 Nov-Dec;17(6):763-71. doi: 10.1111/j.1524-475X.2009.00543.x. PMID: 19903300; PMCID: PMC2810192.
[2] Phillips CJ, Humphreys I, Fletcher J, Harding K, Chamberlain G, Macey S. Estimating the costs associated with the management of patients with chronic wounds using linked routine data. Int Wound J. 2016 Dec;13(6):1193-1197. doi: 10.1111/iwj.12443. Epub 2015 Mar 26. PMID: 25818405; PMCID: PMC7949824.
[3] Purwins S, Herberger K, Debus ES, Rustenbach SJ, Pelzer P, Rabe E, Schäfer E, Stadler R, Augustin M. Cost-of-illness of chronic leg ulcers in Germany. Int Wound J. 2010 Apr;7(2):97-102. doi: 10.1111/j.1742-481X.2010.00660.x. PMID: 20529149; PMCID: PMC7951196.
[4] Yammine K, El Alam A, Alqaysi B, Assi C. The internal pedal amputation as a salvage procedure in diabetic and ischemic foot infection. A meta-analysis. Foot Ankle Surg. 2022 Feb;28(2):159-165. doi: 10.1016/j.fas.2021.03.008. Epub 2021 Mar 16. PMID: 33752981
[5] Reitan RL, McBroom RM, Gilder RE. The Risk of Infection and Indication of Systemic Antibiotics in Chronic Wounds. Wounds. 2020 Jul;32(7):186-194. PMID: 33166266.
[6] Schollemann F, Kunczik J, Dohmeier H, Pereira CB, Follmann A, Czaplik M. Infection Probability Index: Implementation of an Automated Chronic Wound Infection Marker. J Clin Med. 2021 Dec 29;11(1):169. doi: 10.3390/jcm11010169. PMID: 35011910; PMCID: PMC8745914
[7] Malone M, Bjarnsholt T, McBain AJ, James GA, Stoodley P, Leaper D, Tachi M, Schultz G, Swanson T, Wolcott RD. The prevalence of biofilms in chronic wounds: a systematic review and meta-analysis of published data. J Wound Care. 2017 Jan 2;26(1):20-25. doi: 10.12968/jowc.2017.26.1.20. PMID: 28103163.
[8] Honorato-Sampaio K, Guedes AC, Lima VL, Borges EL. Bacterial biofilm in chronic venous ulcer. Braz J Infect Dis. 2014 May-Jun;18(3):350-1. doi: 10.1016/j.bjid.2014.01.003. Epub 2014 Mar 21. PMID: 24662137
[9] Hurlow J, Bowler PG. Acute and chronic wound infections: microbiological, immunological, clinical and therapeutic distinctions. J Wound Care. 2022 May 2;31(5):436-445. doi: 10.12968/jowc.2022.31.5.436. PMID: 35579319.
[10] Costerton JW, Stewart PS, Greenberg EP. Bacterial biofilms: a common cause of persistent infections. Science. 1999 May 21;284(5418):1318-22. doi: 10.1126/science.284.5418.1318. PMID: 10334980.
[11] Kingsley A. The wound infection continuum and its application to clinical practice. Ostomy Wound Manage. 2003 Jul;49(7A Suppl):1-7. PMID: 12883156.
[12] Deeth M. A closer look at the wound infection continuum. Br J Community Nurs. 2017 Dec 1;22(Sup12):S48-S50. doi: 10.12968/bjcn.2017.22.Sup12.S48. PMID: 29189070.
[13] Gottrup F. A specialized wound-healing center concept: importance of a multidisciplinary department structure and surgical treatment facilities in the treatment of chronic wounds. Am J Surg. 2004 May;187(5A):38S-43S. doi: 10.1016/S0002-9610(03)00303-9. PMID: 15147991.
[14] Falcone M, De Angelis B, Pea F, Scalise A, Stefani S, Tasinato R, Zanetti O, Dalla Paola L. Challenges in the management of chronic wound infections. J Glob Antimicrob Resist. 2021 Sep;26:140-147. doi: 10.1016/j.jgar.2021.05.010. Epub 2021 Jun 16. PMID: 34144200.
[15] Brun-Buisson C. The epidemiology of the systemic inflammatory response. Intensive Care Med. 2000;26 Suppl 1(Suppl 1):S64-74. doi: 10.1007/s001340051121. PMID: 10786961; PMCID: PMC7094973
[16] Naude L. The use of Prontosan® in combination with Askina® Calgitrol®: an independent case series. Wounds International 2018; 9 (1): 44-8. Brun-Buisson C. The epidemiology of the systemic inflammatory response. Intensive Care Med. 2000;26 Suppl 1(Suppl 1):S64-74. doi: 10.1007/s001340051121. PMID: 10786961; PMCID: PMC7094973
[17] Christaki E, Marcou M, Tofarides A. Antimicrobial Resistance in Bacteria: Mechanisms, Evolution, and Persistence. J Mol Evol. 2020 Jan;88(1):26-40. doi: 10.1007/s00239-019-09914-3. Epub 2019 Oct 28. PMID: 31659373.
[18] Dhingra S, Rahman NAA, Peile E, Rahman M, Sartelli M, Hassali MA, Islam T, Islam S, Haque M. Microbial Resistance Movements: An Overview of Global Public Health Threats Posed by Antimicrobial Resistance, and How Best to Counter. Front Public Health. 2020 Nov 4;8:535668. doi: 10.3389/fpubh.2020.535668. PMID: 33251170; PMCID: PMC7672122.
[19] Samreen, Ahmad I, Malak HA, Abulreesh HH. Environmental antimicrobial resistance and its drivers: a potential threat to public health. J Glob Antimicrob Resist. 2021 Dec;27:101-111. doi: 10.1016/j.jgar.2021.08.001. Epub 2021 Aug 25. PMID: 34454098.
[20] Pires D, de Kraker MEA, Tartari E, Abbas M, Pittet D. ‘Fight antibiotic resistance—it’s in your hands’: call from the World Health Organization for 5th May 2017. Clin Infect Dis 2017;64:1780–3. doi: 10.1093/cid/cix226 .
[21] O’Neill J. Review on Antimicrobial Resistance. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations. 2014. https://amr-review.org/Publications.html. Accessed July 12, 2023.